Preventing Dehydration in Kids During Illness or Activities

Does anyone else spend a good part of their day chasing their kids with water bottles, telling them, "Don't forget to drink this!" or gathering six nearly full water bottles rattling around on the car floor? Or is it just me?
We all know we need to stay hydrated, and we also know that getting kids to drink water when they're busy or when they'd rather have juice, soda, or literally anything else can be tricky! Just look at the water bottle graveyard in my car for proof.
Staying well-hydrated is even more important when children are sick, it's very hot outside, or they're engaging in extended play or sports sessions. Dehydration, which occurs when the body lacks sufficient water, can occur much more quickly in children than in adults, especially during fever, vomiting, diarrhea, or prolonged activity.
In this blog, we'll discuss hydration strategies for illness or physical activity, when electrolyte solutions are helpful, and how to recognize early warning signs of dehydration in babies, toddlers, and school-aged kids.
Understanding Normal Hydration Needs for Kids
Children need regular access to water throughout the day to support hydration, digestion, temperature regulation, and healthy immune function. According to the American Academy of Pediatrics, water is the best everyday drink for children and should be offered routinely at meals, snacks, and during play!
In terms of hydration strategies for kids, most school-aged children do well with steady sips of water throughout the day rather than large amounts at once. The same goes for toddlers - they should have water offered with meals and available during the day.
The goal is to drink enough water so you don't feel thirsty! Thirst is an early sign of dehydration.
Babies get hydration from formula or breastmilk, and following a nursing-on-demand schedule or offering age-appropriate volumes of formula every few hours is usually the perfect way to keep your child hydrated.
During times of rest and good health, instead of worrying too much about the total amount of water your child drinks, watch their urine color. A child’s urine color is often a helpful indicator: pale yellow means they are well-hydrated, while darker yellow may mean they need more fluids.
For babies, the color of urine is hard to see, but they should have plenty (at least 4) of good wet diapers, have moist mouths and lips, and appear otherwise well.
Dehydration During Illness: What Parents Need to Know
Illness-related dehydration is one of the most common reasons families seek medical care. When kids get sick from illnesses like the flu or stomach bugs like norovirus, dehydration is a leading cause of hospital visits.
Vomiting, diarrhea, and fever can all increase fluid loss and make it harder for children to stay hydrated. Being sick can raise a child's heart and respiratory rates, and, combined with a higher core temperature (a fever), can cause the child to use up available fluids quickly, leading to dehydration.
This is perpetuated by the fact that kids don't feel well and are therefore less likely to keep drinking water to maintain their hydration. Colds and runny noses, especially in babies, can also cause fluid to escape.
Common sense tells us that vomiting and diarrhea lead to fluid loss, which causes dehydration. This is supported by research showing that children can become dehydrated quickly when gastrointestinal symptoms occur, and that early treatment with electrolyte solutions is crucial.
How dehydration develops during illness
- Vomiting causes immediate fluid and electrolyte loss.
- Diarrhea may lead to significant fluid losses, especially in infants.
- Fever increases water needs because children breathe faster, their heart rate can go up, and they may sweat more.
- Poor intake from decreased appetite or nausea makes it harder to replace losses.
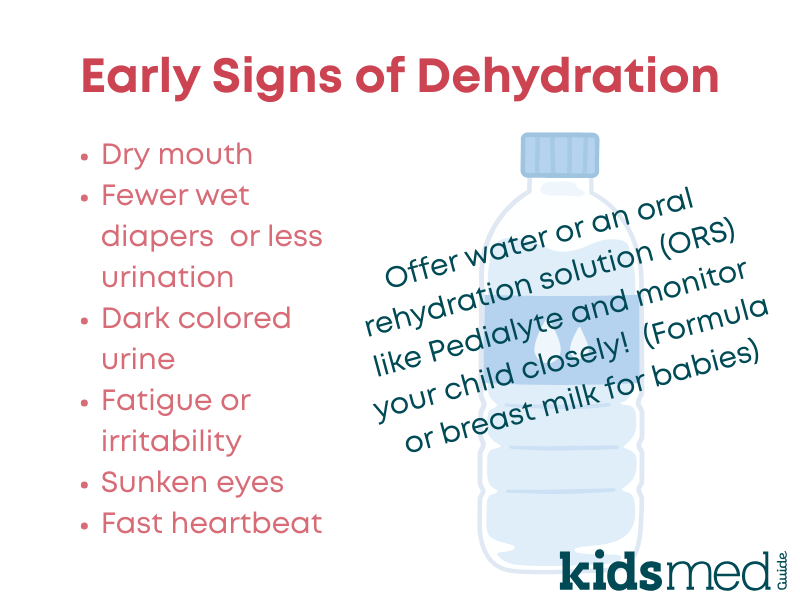
Signs of dehydration to watch for
- Dry mouth or cracked lips
- Fewer wet diapers or infrequent urination
- No tears when crying
- Lethargy, irritability, or unusual sleepiness
- Sunken eyes
- Sunken soft spot (fontanelle) in babies
- Fast heartbeat
- Cool hands and feet
Using Oral Electrolyte Solutions Safely
When dehydration occurs or when you're actively trying to prevent it, you might consider using an oral rehydration solution (ORS) — something like Pedialyte® or Gatorade®, and it's very helpful to keep on hand! (I've been to the drugstore at 11 PM more than once...)
Pedialyte® is one of the best products and my preferred brand, because it contains the most helpful and necessary electrolytes, with the right balance of water, salts, and sugars, which is ideal for kids, and it has the least amount of unnecessary extras.
Evidence supports the use of oral rehydration solutions (ORS) as the standard treatment for mild to moderate dehydration. These solutions contain the right mix of water, sodium, glucose (sugar), and other minerals for quick absorption. Even better, they can be administered at home and don't need a doctor or an IV!
Plain water alone is not enough in the setting of dehydration caused by diarrhea or vomiting, as children also lose sodium, sugar, and other electrolytes necessary for fluid balance.
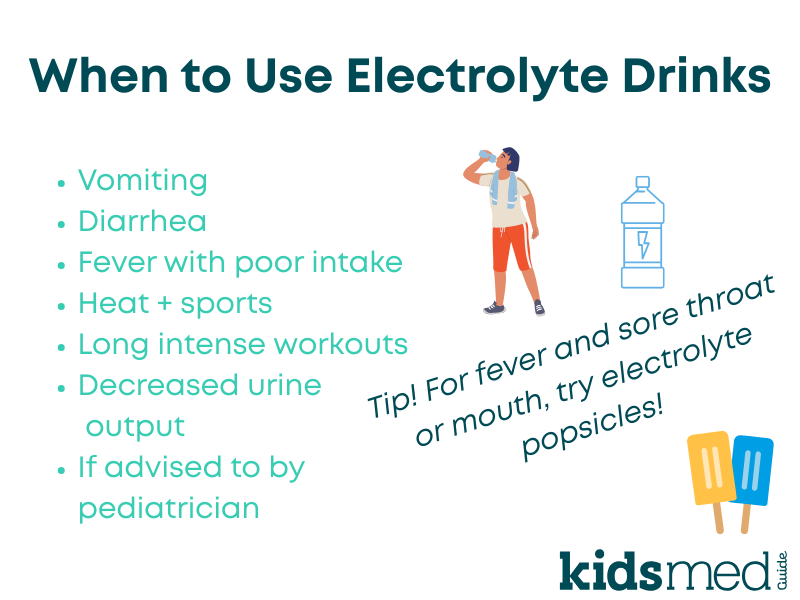
When to use electrolyte solutions
- Vomiting or diarrhea lasting more than a few hours
- Any illness with reduced food and water intake
- Fever accompanied by poor drinking
- Anytime urine output decreases
- Periods of intense physical activity, especially if outdoors in the heat
How to give electrolyte solutions
Offer small amounts every 5 to 10 minutes for younger children. Older children should take slow sips rather than large gulps to reduce the chance of vomiting.
Our hot tip? Keep a variety of Pedialyte® options on hand in your home at all times! They come in jugs, single-serve packets, and freeze pops.
Hydration Considerations for Babies
Infants are at the highest risk of dehydration because their fluid reserves are smaller and they lose water more quickly. There's an old saying that babies are "little bags of water," and it's true!
Physiologically, babies have a higher water content than older children and adults, which makes them more susceptible to the negative effects of water loss.
Babies can also lose water in all kinds of ways - peeing, pooping, vomiting, runny noses, refusal to nurse or bottlefeed, faster heart and respiratory rates - and these all may get more significant during times of illness.
Breastfed babies
Breastfeeding should continue during illness. Breastmilk provides hydration, immune support, and easily absorbed nutrients. Babies should ideally be allowed to nurse as long and often as they want when they are ill, although speak with your pediatrician about offering small volumes of milk if your child is acutely vomiting with a viral gastroenteritis.
Formula-fed babies
Continue regular formula feeding unless instructed otherwise by the pediatrician. You may consider increasing formula intake if your baby seems dehydrated (fewer wet diapers) or if you suspect they are losing more fluids than usual through stool or other secretions, such as a runny nose.
If your child is acutely ill and vomiting from something like a viral gastroenteritis, offer formula in small quantities until the acute vomiting phase has passed - read more in our norovirus guide.
Babies younger than six months should not receive water or electrolyte drinks unless directed by a medical professional.
When babies need medical evaluation
- Fewer than three wet diapers in 24 hours
- Constant sleepiness or difficulty waking
- Dry mouth
- Sunken soft spot (fontanelle)
- Persistent vomiting
Emergency signs of dehydration: If your child is so lethargic (sleepy) that they can't be woken up, or is breathing rapidly or slowly, or appears blue, cold, or mottled around the mouth, or if their heart rate is too rapid or too slow, or if any symptoms are alarming to you, call 911 or take them to the emergency room.

Hydration During Sports, Heat, and High Activity
Physical activity causes fluid loss mainly through sweat. Some fluid is also lost through muscle exertion and increased metabolic rates, but sweat is the primary route!
Often, kids who are exercising don't realize they are becoming dehydrated. Long practices, outdoor play, and warm weather increase the risk of dehydration and electrolyte imbalance.
Heat + sun + physical activity = increased risk of dehydration.
Key hydration strategies for active kids
- Encourage drinking water before, during, and after activity. Don't start dehydrated.
- Provide scheduled water breaks, and enforce them!
- Use lightweight reusable bottles that kids can easily fill up as needed.
- Offer fruits like oranges or watermelon during and after activity.
- For very high-intensity workouts or very hot days, consider using water and an oral rehydration solution (ORS), such as Pedialyte® or Gatorade®.
Preventing Dehydration at Home
Try to prevent dehydration before it begins, because it can make kids (and adults) feel really terrible! It can also become so serious that they can get critically ill or need an emergency room visit for IV fluids.
Here are some tips to stay hydrated each day:
- Offer water consistently, and remind children to drink it
- Provide water-rich foods such as berries and cucumbers
- Encourage slow, steady drinking
- Use kid-friendly cups or bottles
- Model good hydration habits yourself - use that Stanley®!
- Try to avoid sugary treats like juice and soda, because kids will naturally prefer that over water, which is the gold standard
- Periodically check in on your child's urination habits - are they going several times a day, and is the color clear to pale yellow?
Emergency Signs of Dehydration: When to Seek Medical Care
Seek emergency care if your child has:
- Severe vomiting or inability to keep fluids down
- Lethargy or unresponsiveness
- No urination for eight or more hours
- Sunken eyes or fontanelle
- Bloody diarrhea
- Fast breathing or heartbeat
- Cool or mottled skin
- Persistent high fever with poor intake
Frequently Asked Questions
How much should my child drink each day?
Pale yellow urine is a good sign of hydration. Needs vary by age and activity.
Should I offer water or electrolyte drinks first during illness?
Electrolyte solutions are recommended when vomiting or diarrhea occurs, because they help replace sodium, glucose, potassium, and other electrolytes along with water.
Are electrolyte drinks safe for babies?
Babies younger than six months should not be given electrolyte drinks unless advised by a pediatrician. They should rehydrate with breastmilk or formula. Consult your pediatrician for guidance on managing dehydration in infants.
When should kids use electrolyte drinks during sports?
Electrolyte drinks are helpful for activities lasting over 1 hour or for intense workouts in warm weather.
Can homemade oral rehydration solutions work?
Commercial ORS products like Pedialyte® or Gaotrade® have precise sodium-to-glucose ratios designed for optimal absorption, and are preferred for safety.
The following references were used to compile this information:
Breastfeeding Benefits Your Baby’s Immune System. (2023, August 30). HealthyChildren.Org. https://www.healthychildren.org/English/ages-stages/baby/breastfeeding/Pages/Breastfeeding-Benefits-Your-Babys-Immune-System.aspx
Choose Water for Healthy Hydration. (2024, July 26). HealthyChildren.Org. https://www.healthychildren.org/English/healthy-living/nutrition/Pages/Choose-Water-for-Healthy-Hydration.aspx
Dehydration: Giving Liquids at Home. (n.d.). Retrieved November 13, 2025, from https://www.nationwidechildrens.org/conditions/dehydration
Dehydration in Kids. (n.d.). Retrieved November 13, 2025, from https://www.luriechildrens.org/en/blog/dehydration-in-children/
Hartman, S., Brown, E., Loomis, E., & Russell, H. A. (2019). Gastroenteritis in Children. American Family Physician, 99(3), 159–165.
Hydration | Boston Children’s Hospital. (n.d.). Retrieved November 13, 2025, from https://www.childrenshospital.org/treatments/hydration
Imdad, A., & Rani, U. (2025). Oral Rehydration Salt Solutions for Children: A Review. Pediatrics In Review, 46(7), 355–365. https://doi.org/10.1542/pir.2024-006404
Kannikeswaran, N. (2024). Dehydration. Pediatric Care Online. https://doi.org/10.1542/aap.ppcqr.396249
Managing Acute Gastroenteritis Among Children: Oral Rehydration, Maintenance, and Nutritional Therapy. (n.d.). Retrieved November 13, 2025, from https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5216a1.htm
Recommended Drinks for Children Age 5 & Younger. (2023, October 3). HealthyChildren.Org. https://www.healthychildren.org/English/healthy-living/nutrition/Pages/recommended-drinks-for-young-children-ages-0-5.aspx
Signs of Dehydration in Infants & Children. (2019, September 24). HealthyChildren.Org. https://www.healthychildren.org/English/health-issues/injuries-emergencies/Pages/dehydration.aspx
Signs of Dehydration in Kids and How To Prevent It. (n.d.). Cleveland Clinic. Retrieved November 13, 2025, from https://health.clevelandclinic.org/signs-of-dehydration-in-kids
Sports Nutrition for Busy Families and Busy Lifestyles. (2017, March 6). HealthyChildren.Org. https://www.healthychildren.org/English/healthy-living/nutrition/Pages/Sports-Nutrition-for-Busy-Families-and-Busy-Lifestyles.aspx
Treating Dehydration with Electrolyte Solution. (2023, February 6). HealthyChildren.Org. https://www.healthychildren.org/English/health-issues/conditions/abdominal/Pages/Treating-Dehydration-with-Electrolyte-Solution.aspx



